BY DAKSHITA NAITHANI
INTRODUCTION
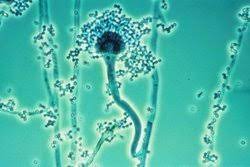
Pier Antonio Micheli, a priest and scientist, named Aspergillus while documenting moulds in 1729. The mould looked like an aspergillum, which is a type of holy water sprinkler. Physician Georg W. Fresenius described the species fumigatus for the first time in 1863.
Apergillus spp., found in abundance of nature, can be found in soil, decomposing materials, water sources, and air particle. Aspergillus-related disease is uncommon, although it has a significant death rate. The majority of people are exposed to spores (conidia) during their lives, although illness development occurs mostly in people with compromised immune systems, as well as during construction and yard activities. In patients with leukaemia, asthma, cystic fibrosis, and hematopoietic stem cell transplant recipients, A.fumigatus is the most frequent invasive mould infection, with death rates exceeding 50 percent in these high-risk populations.
Around the apex, the stipes are grey in colour. They feature a slick finish. Their globule is tiny and columnar. The conidia’s texture is either smooth or spinose.
WHERE IT CAN BE FOUND?
Aspergillus is commonly found in rotting plant matter. After considerable environmental exposure to Aspergillus spores, such as when handling tree-bark chipping, Aspergillosis can develop in healthy hosts.
Aspergillus can be found in soil, compost piles, and damp grain in outdoor settings. Aspergillus may be found within buildings in wet insulation, fireproofing material, beds , behind couches, in damp rooms’ corners, dust, and air conditioning systems. In the Northern Hemisphere, most research studying seasonal changes in fungal exposure show an increase in airborne Aspergillus throughout the cold season.
TYPES OF ASPERGILLOSIS
Allergic bronchopulmonary aspergillosis (ABPA) is a multifaceted hypersensitivity reaction to inhaled Aspergillus fumigatus. Although it produces lung irritation and allergy symptoms, it does not cause infection. Aspergillus sinusitis is caused by an allergic reaction to the fungus Aspergillus, which produces inflammation in the sinuses and the symptoms of a sinus infection but does not cause an infection. A fungus ball is also known as an Aspergilloma. It forms in the lungs or sinuses but seldom spreads to other regions of the body, as the name implies.
Aspergillosis of the lungs (chronic pulmonary aspergillosis) Aspergilloma, chronic cavitary pulmonary aspergillosis (CCPA), chronic fibrosing pulmonary aspergillosis (CFPA), and Aspergillus nodules are all illnesses classified as chronic pulmonary aspergillosis (CPA). CPA is a lung infection that develops over time.
INVASIVE PULMONARY ASPERGILLOSIS
Inhaled conidia are removed by epithelial cells and alveolar macrophages in normal host lungs. Aspergillus becomes invasive when conidia escape these host defences and develop into branching filaments called hyphae. Alveolar macrophages generate inflammatory mediators, which attract neutrophils, which can destroy the hyphae.
CUTANEOUS SKIN ASPERGILLOS
Aspergillus comes in contact through a breach in the skin (for example, after surgery or a burn wound) and infects persons with weaker immune systems. Cutaneous Aspergillosis can also develop if invasive Aspergillosis moves from another part of the body, such as the lungs, to the skin.
LIFE CYCLE
Aspergillus begins its infectious life cycle by producing conidia (asexual spores) that are easily transported into the atmosphere, ensuring its ubiquity in both habitats. Inhalation of these conidia is the most common way to become infected, followed by conidial deposition in the bronchiole spaces. The phagocytosis and destruction of Aspergillus conidia is largely carried out by macrophages. The danger of infection stems largely from a breakdown in these host defences, as well as fungal characteristics that allow A. fumigatus to survive and flourish in this pulmonary habitat.
SYMPTOMS
The symptoms of Aspergillosis are:
- Wheezing, chest pain
- Shortness of breath, stuffiness, runny nose and reduced ability to smell
- Cough (sometimes blood)
- Fever (in rare cases), headache, fatigue
- Weight loss
• The length of time that an illness lasts depends on the underlying health concerns, the intensity or location of infection, and the kind of sickness.
• Allergic forms, may require steroid and antifungal treatment for a few months, possibly longer sometimes.
• Invasive pulmonary Aspergillosis may need at least 6 to 12 weeks of antifungal therapy. Severe cases may need therapy for lifetime and monitoring to keep the illness under control.
• If the infection spreads from the lungs to other areas of the body, additional symptoms may appear.
• Red to purple plaques or papules are common symptoms of cutaneous Aspergillosis.
DIAGONOSIS
Because the symptoms of Aspergillosis might be confused with those of other lung diseases, diagnosing it can be challenging. In order to make a diagnosis, your healthcare practitioner will look at your medical history, risk factors, symptoms, physical examinations, and lab testing.
An Aspergilloma, a fungal tumour, or the symptoms of invasive Aspergillosis and ABPA can be found on a chest X-Ray or a chest CT scan.
• A sample of your sputum is stained with a dye and examined for the presence of Aspergillus filaments in a respiratory secretion (sputum) test.
• Tissue and blood testing may be used to confirm the presence of ABPA.
• To confirm invasive aspergillosis, a biopsy of tissues from your lungs or sinuses is performed, as well as blood testing.
TREATMENT
In addition to early diagnosis, early treatment is critical in managing aspergillosis. Depending on the type of disease, one may have the following treatments:
• Observation- If you have a single aspergilloma, you may not need treatment; instead, you may be monitored with regular chest X-rays or CT scans. The doctor may prescribe antifungal medication if your disease worsens.
• Antifungal medicines may be used in combination with corticosteroids to reduce the need of steroids, improve lung function, and prevent existing asthma or cystic fibrosis from deteriorating. Some examples are prednisone (Deltasone), prednisolone (Orapred), and methylprednisolone (Medrol).
• Invasive pulmonary aspergillosis is treated with antifungal medications. Voriconazole (VFEND) and amphotericin B are two of these drugs (Amphocin, Fungizone).
• Surgery- as antifungal medicines have a hard time penetrating an aspergilloma, surgery may be required to remove the fungal mass if the aspergilloma causes pulmonary haemorrhage.
Embolization of the Arteries -This technique can be used to temporarily halt aspergilloma-related bleeding. A radiologist uses a catheter to inject a substance into an artery supplying a lung cavity where an aspergilloma is causing blood loss. The injected substance solidifies, cutting off the area’s blood supply and halting the bleeding. This therapy works for a while, but the bleeding will most likely return.


You must be logged in to post a comment.