Smallpox-like lesions spotted on Ancient Egyptian mummies reveal that the nasty disease has been there for the past 3,000 years and remained one of the world’s most dreadful diseases until a global vaccination programme spearheaded by the World Health Organization wiped it off. In the 4th century CE, the first documented mention of smallpox-like sickness emerged in China. In the 7th century, early written accounts arose in India, and in the 10th century, they appeared in Asia Minor.
In 1977, the last confirmed natural case occurred in Somalia. Ever since, the only documented cases can be traced back to a laboratory mishap in Birmingham, England, in 1978, which claimed one life and resulted in a small breakout. In 1980, the World Health Organization declared smallpox eradicated. On average, three out of every ten people who contracted it succumbed. Those who survived suffered permanent scars.
INITIAL TREATMENT OF SMALLPOX
Smallpox was 60 times more lethal as prevailing Covid-19 and twice as contagious. It tormented humanity for millennia, blinding and scarring many survivors, and killing roughly 300-500 million people in the twentieth century alone.
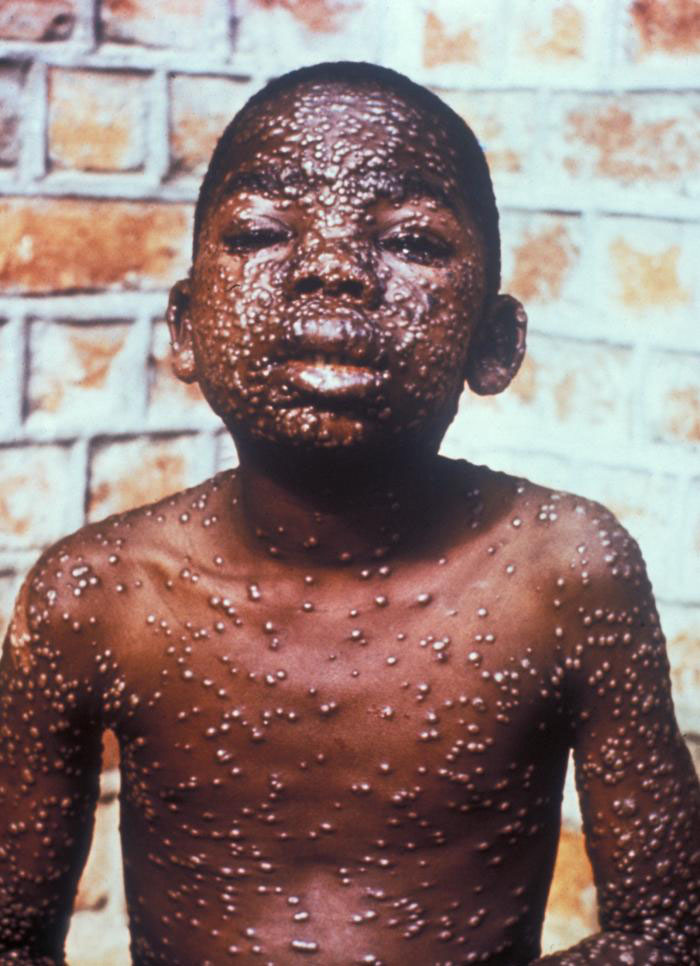
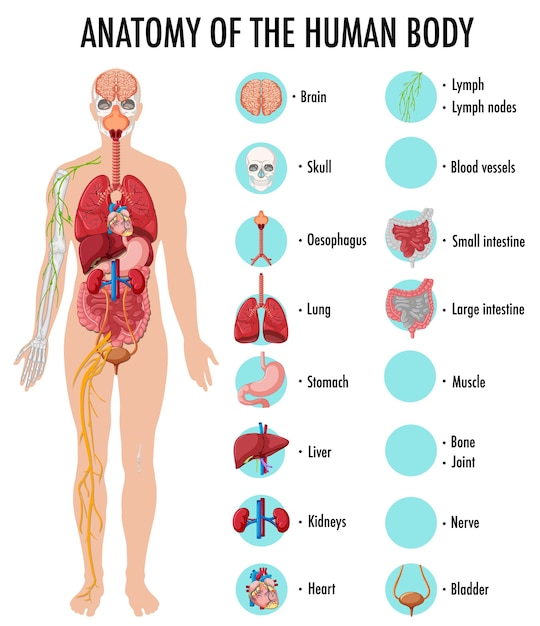
The variola virus causes smallpox. Early signs and symptoms include a high fever and weariness. The disease then induces a rash, most noticeable on the face, arms, and legs. The ensuing lesions swell with clear fluid, then pus, and eventually form a crust, which dries up and comes off.
Variolation, a process dubbed after the variola virus that causes smallpox, was one of the earliest treatments for controlling the disease. People who had never had smallpox were exposed to matter from smallpox sores during variolation by scratching it into their arm or inhaling it via their nose. People acquired smallpox-like symptoms following variolation, like fever and a rash. Variolation was not completely effective; up to 3% of persons died after being subjected to the puss.

In 1796, English doctor Edward Jenner established the cornerstone for vaccination when he observed that cowpox-infected milkmaids were immune to smallpox. The cowpox virus is a member of the Orthopoxvirus family, which also includes the variola virus that causes smallpox.
Dr. Jenner put his idea to the test by inoculating James Phipps, Jenner’s gardener’s 9-year-old son, with matter from a cowpox lesion on milkmaid Sarah’s hand. James had a single blister on the spot, but he recovered quickly. Jenner frequently subjected Phipps to the variola virus, but Phipps never obtained smallpox. The vaccine was effective. Doctors all around Europe quickly embraced Jenner’s ground-breaking procedure, resulting in a significant reduction in new cases of the dangerous illness.
SMALLPOX ERADITION
All Developed nations had huge success in eradicating Smallpox with mass vaccination campaigns; yet, developing countries had to adopt a different strategy. ‘Surveillance and containment’ were the term for this strategy. Intense house-to-house screenings and incentives for people who reported smallpox cases assisted surveillance. Ring vaccination and isolation of patients and everyone who had come into touch with them was among the containment strategies.
India represented almost 60% of the world’s reported cases of smallpox in the early 1960’s. Many cases went unreported because of the stigma associated with the disease. The strain of smallpox found in India was much deadlier than strains found in West Africa. The Indian Government introduced NSEP in 1962, the National Smallpox Eradication Program aimed at mass population vaccination. Money was invested & inoculation workers were employed. Around 60 million vaccines were administered by 1966, along with 440 million re-vaccinations.
By 1967, however, smallpox cases were growing in India, indicating the failure of the vaccination campaign. One of the greatest reasons being individual reluctance and refusal to participate in the vaccination programs, because of lack of trust in the vaccines or religious beliefs. The method of vaccination was also a problem. Before 1969, a drop of the vaccine was placed on the person’s arm and pushed into the skin with a single-point needle. This procedure was repeated for primary vaccination five times and for revaccination fifteen times.
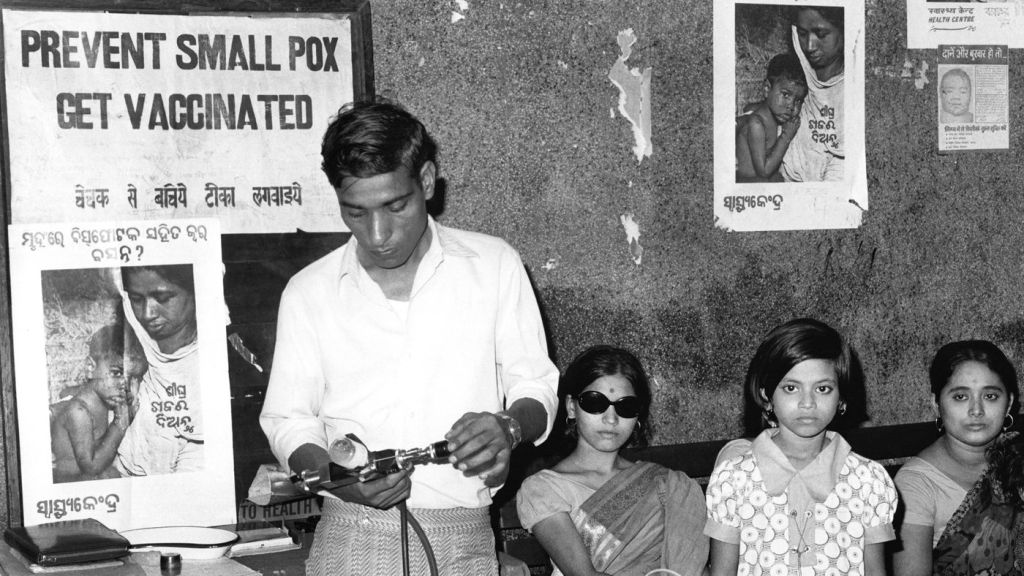
In Sept. 1970, the Indian government and the WHO signed a Plan Of operation The World Health Organization partnership provided India with the opportunity to acquire better-quality freeze-dried vaccines. The jet injector swapped the standard single-point needle and did not require power. Frequent maintenance was essential for the device. The bifurcated needle was a cheaper and quicker vaccination method. For health professionals, minimal level training was needed. For the people, it was less painful.
Vaccinating 80 % of the population in 5 years was deemed adequate to avert smallpox transmission in smaller countries. But the high numbers of births each year (25 million new babies) made this target unfeasible in heavily populated countries like India. It wasn’t enough to contain smallpox.
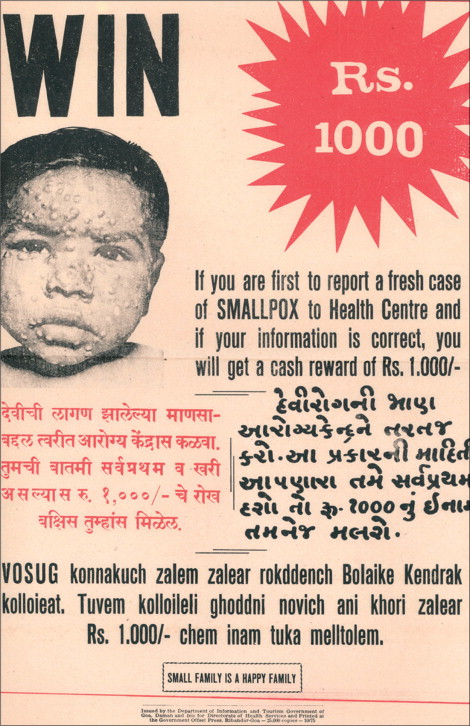
The Indian Government put full force in the National Smallpox Eradication Program. A prize of 1000 rupees for reporting new cases of pox was the most unique but highly successful strategy implemented. The general public reported 11% of outbreaks of smallpox in 1975, as compared with 2.6% in 1973. To encourage vaccination, posters were crafted in native languages, showcasing young children.
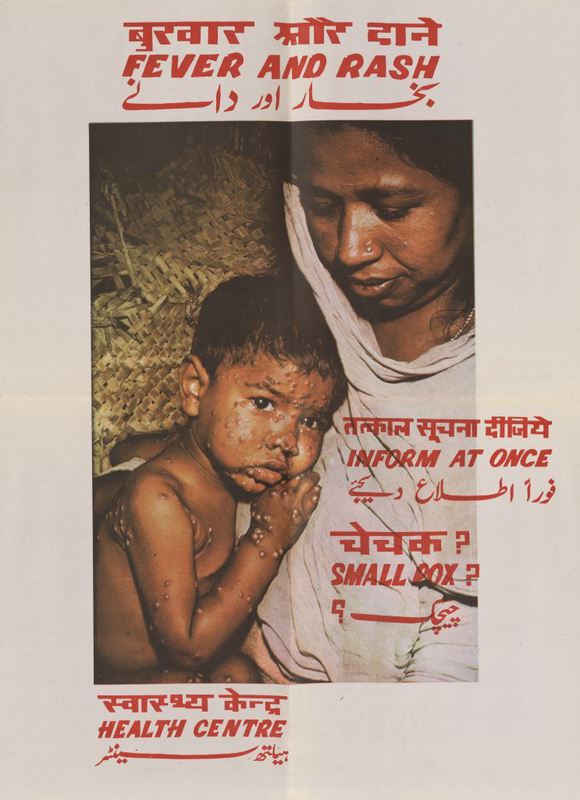
The “surveillance-containment” strategy was straightforward. Healthcare professionals would actively look for possible cases of pox. Affected persons and their families or neighbors would be sequestered and vaccinated right away. To eradicate smallpox, active searches and detection and the control of disease outbreaks were necessary. 110 million houses were searched for new smallpox cases from March to November 1976 in over half a million Indian villages, and in 260 urban areas. Merely 5 cases of chickenpox were discovered.
The International Commission for Eradication Assessment of Smallpox visited the India in April 1977, conducting its own field assessments along with an analysis of the country’s documented evidence. Finally, the International Commission certified India Smallpox free.



You must be logged in to post a comment.