By Eduindex News
Socio-Cultural Factors and Attitudes Affecting the Health Status of Rural Communities
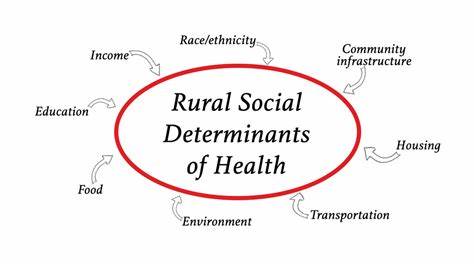
Health is a multidimensional concept influenced by biological, environmental, and socio-cultural factors. Among rural communities, socio-cultural factors and attitudes often play a crucial role in determining health outcomes. These factors are deeply embedded in the social fabric and cultural norms of rural societies, influencing health behaviors, access to healthcare, and overall well-being. Understanding these influences is critical for designing effective health interventions and policies tailored to rural populations.
1. Socio-Cultural Factors Influencing Health
1.1 Traditional Beliefs and Practices
Many rural communities rely on traditional health practices and remedies passed down through generations. While some of these practices may be beneficial, others can hinder timely medical intervention. For instance:
- Faith in Folk Healers: Many rural residents consult local healers or shamans before seeking formal medical care, delaying diagnosis and treatment.
- Herbal Remedies: Although some herbal remedies are effective, unregulated use can lead to complications or interfere with prescribed treatments.
1.2 Gender Norms and Roles
Gender dynamics significantly affect health outcomes in rural areas:
- Maternal Health Neglect: Women’s health, particularly during pregnancy and childbirth, is often deprioritized due to traditional gender roles.
- Limited Autonomy: In patriarchal rural settings, women may lack the authority to seek healthcare independently, exacerbating health issues.
- Preference for Male Children: This can lead to neglect of the nutritional and healthcare needs of female children, affecting their long-term health.
1.3 Literacy and Education
Low literacy rates and lack of health education are major barriers to improving rural health:
- Limited Awareness: Poor understanding of hygiene, nutrition, and disease prevention leads to high incidences of preventable illnesses.
- Misinformation: Superstitions and myths about diseases like tuberculosis or HIV/AIDS further stigmatize affected individuals and impede treatment.
1.4 Social Hierarchies and Caste
Caste-based discrimination and social hierarchies can restrict access to healthcare for marginalized groups:
- Healthcare Disparities: Lower-caste individuals may face discrimination at healthcare facilities or hesitate to seek care due to perceived inferiority.
- Social Exclusion: Fear of ostracism often discourages marginalized communities from addressing sensitive health issues.
2. Attitudes Toward Health and Healthcare
2.1 Perceptions of Illness
Cultural perceptions of illness influence how rural communities respond to health problems:
- Fatalistic Attitudes: Many believe illnesses are a result of fate, divine punishment, or witchcraft, leading to resignation and inaction.
- Stigma: Diseases like leprosy, mental illness, and sexually transmitted infections are often stigmatized, preventing individuals from seeking treatment.
2.2 Preference for Traditional Over Modern Medicine
Resistance to modern medicine is prevalent due to:
- Mistrust of Modern Healthcare: Skepticism toward doctors and hospitals arises from lack of familiarity, previous negative experiences, or perceived high costs.
- Accessibility Issues: Long distances to healthcare facilities and inadequate transportation reinforce dependence on local remedies.
2.3 Attitudes Toward Preventive Care
Preventive healthcare is often undervalued in rural communities:
- Low Vaccination Rates: Misinformation and fear of side effects reduce vaccine uptake.
- Neglect of Routine Checkups: Seeking healthcare is often reserved for emergencies, neglecting preventive measures like regular screenings.
3. Structural Challenges and Their Socio-Cultural Impact
3.1 Limited Healthcare Infrastructure
Inadequate healthcare facilities and professionals in rural areas amplify the socio-cultural barriers to health:
- Scarcity of Female Healthcare Workers: Cultural norms may prevent women from consulting male doctors, reducing access to maternal and reproductive healthcare.
- Overburdened Systems: Overcrowded and understaffed facilities lead to long wait times, further discouraging rural residents from seeking care.
3.2 Poverty and Economic Constraints
Economic hardship intensifies socio-cultural barriers:
- Healthcare Costs: The high cost of modern medical treatments often drives rural residents toward cheaper, traditional alternatives.
- Opportunity Costs: Rural families may prioritize daily wage labor over addressing health issues, leading to delayed care.
3.3 Government and NGO Interventions
While initiatives like mobile health clinics and telemedicine aim to bridge gaps, their effectiveness is often limited by:
- Cultural Mismatch: Programs not tailored to local beliefs and practices face resistance.
- Lack of Community Involvement: Exclusion of local leaders and influencers from planning processes reduces program acceptance.
4. Strategies to Improve Rural Health Outcomes
4.1 Promoting Health Education
- Awareness Campaigns: Using local languages and traditional media to disseminate health information can improve understanding and acceptance.
- School-Based Programs: Introducing health education in rural schools ensures early exposure to preventive healthcare practices.
4.2 Culturally Sensitive Interventions
- Engaging Local Leaders: Collaboration with community elders and religious leaders can build trust and ensure program success.
- Integrating Traditional and Modern Medicine: Recognizing the value of certain traditional practices while promoting evidence-based modern treatments can foster acceptance.
4.3 Empowering Women
- Self-Help Groups: Encouraging women’s groups to discuss health issues and pool resources for medical care can enhance access and awareness.
- Training Female Healthcare Workers: Employing and training women from local communities to provide healthcare can overcome gender-related barriers.
4.4 Strengthening Healthcare Infrastructure
- Decentralized Services: Establishing more primary health centers and mobile clinics can improve accessibility.
- Subsidized Healthcare: Government subsidies for healthcare services and medicines can alleviate financial barriers.
Conclusion
The health status of rural communities is intricately linked to socio-cultural factors and attitudes that influence healthcare behaviors and access. Addressing these challenges requires a holistic approach that combines culturally sensitive health interventions, robust infrastructure, and community empowerment. Policymakers, healthcare providers, and NGOs must work collaboratively to bridge the gap between traditional beliefs and modern healthcare, ensuring equitable and effective health services for rural populations. Only through such inclusive efforts can we hope to achieve sustainable improvements in rural health outcomes.
References
Abdullah, M. A. (1993). Traditional practices and other socio-cultural factors affecting the health of children in Saudi Arabia. Annals of tropical paediatrics, 13(3), 227-232.
Amadi, L., Wordu, S., & Ogbanga, M. (2015). Sustainable Development in Crisis? A Post Development Perspective. Journal of Sustainable Development in Africa, 17(1), 140-163.
Chelogoi, D. N., Jonyo, F. O., & Amadi, H. (2020). The influence of socio-cultural factors in access to healthcare in Kenya: A case of Nairobi County, Kenya. Journal of Social and Political Sciences, 3(3).
Ogbanga, M. M. (2024). Oil, Gender and Unemployment: Social Issues in the Niger. Eduindex.
Riemenschneider, H., Balázs, P., Balogh, E., Bartels, A., Bergmann, A., Cseh, K., … & Voigt, K. (2016). Do socio-cultural factors influence medical students’ health status and health-promoting behaviors? A cross-sectional multicenter study in Germany and Hungary. BMC Public Health, 16, 1-10.
Uzobo, E., Ogbanga, M. M., & Jackson, J. T. C. B. (2014). Socio-cultural factors and attitudes affecting the health status of rural communities: a study of Danmusa, Katsina State, Nigeria. Int J Sci Res, 3(3), 837-844.


You must be logged in to post a comment.