As a parent, it’s sometimes hard to be away from your kids. But it’s an indescribable, heartwarming feeling when you return – their smiles, the running to you with open arms, their tiny arms squeezing your neck. Whether you’ve been gone ten minutes or two days, that moment, this sweet reward, is everything.But what if reunions aren’t possible because the goodbyes are too much for your child to bear? If goodbyes are full of tears and fits, your little one might have separation anxiety.
Separation anxiety is a normal part of development that occurs when toddlers begin to grow more aware and develop stronger relationships with their caregivers. This awareness can make them more apprehensive and possibly feel unsafe without their parent or caregiver.Whether it’s dropping your child off at day-care or leaving your child at home as you head out to work, farewells can be difficult. Your child may understand that mommy and daddy didn’t vanish, but they might not know for how long. All they know is that they feel safest when you’re around.

When does it begin?
Separation anxiety typically develops before age 1 and peters out around age 3, but it can be experienced by older children and young adults as well—particularly during major life changes like transitioning to high school or leaving for college. Certain life stressors can trigger feelings of anxiety about being separated, such as divorce, loss of a pet, new caregiver, a new sibling, a new school or moving to a new place.
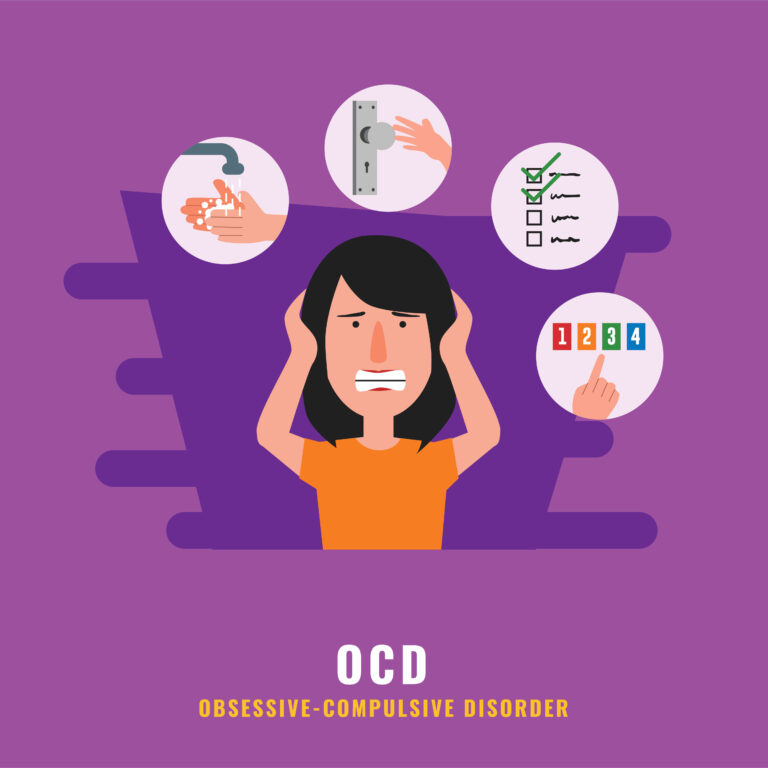
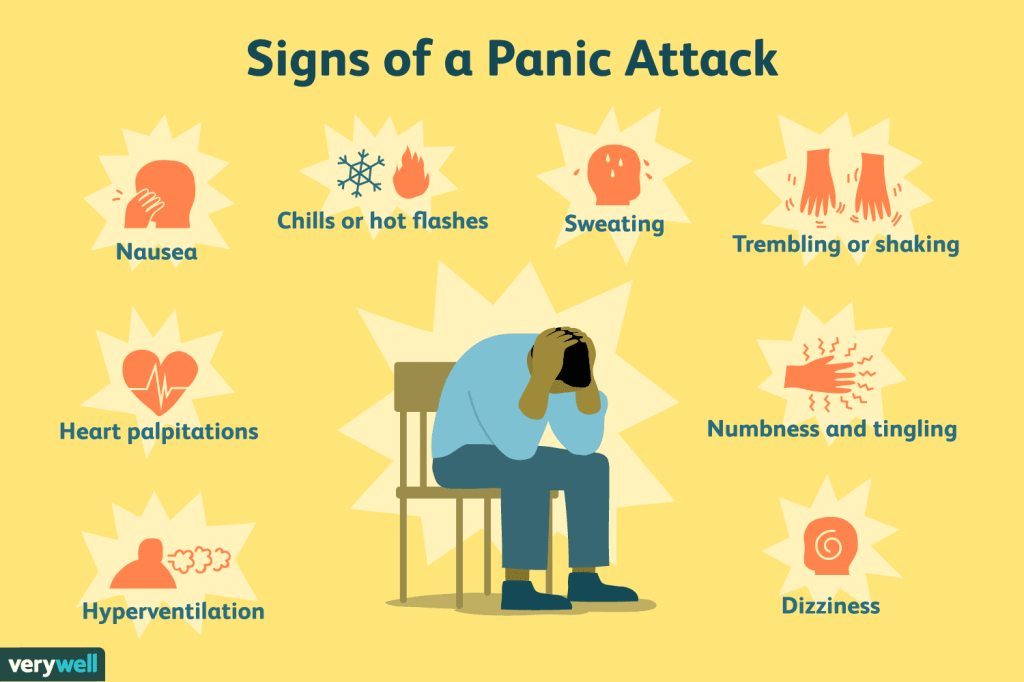
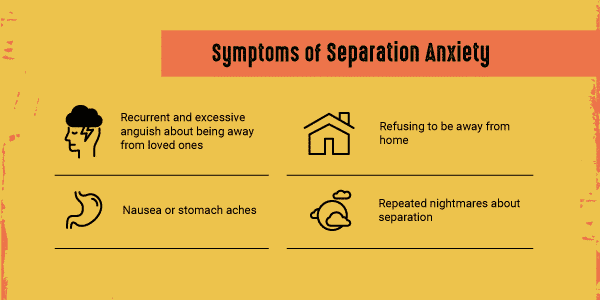
Separation anxiety can be normal and temporary. Although it can be difficult for your child, and for you as their parent, remember this indicates a strong attachment between you and your child.However, if you notice your child’s anxiety starts affecting their daily life and academics, talk to their doctor. Things like stomach aches, vomiting, headaches, constant worry about losing you or a loved one to a disease or illness or a reluctance to sleep away from you may be a sign of a more serious emotional problem called separation anxiety disorder (SAD. The main difference between the two is that with SAD their fears keep them from normal activities. Adult separation anxiety can have an onset in childhood or adulthood. Similar to other anxiety disorders, adult separation anxiety can affect your quality of life, but the condition can be managed with treatment. Talk to a medical professional if you suspect you or someone you love is living with this disorder.

Common causes of separation anxiety disorder
Separation anxiety disorder occurs because a child feels unsafe in some way. Take a look at anything that may have thrown your child’s world off balance, made them feel threatened, or upset their normal routine. If you can pinpoint the root cause—or causes—you’ll be one step closer to helping your child through their struggles.Common causes of separation anxiety disorder in children include:
- Change in environment. Changes in surroundings, such as a new house, school, or day care situation, can trigger separation anxiety disorder.
- Stress. Stressful situations like switching schools, divorce, or the loss of a loved one—including a pet—can trigger separation anxiety problems.
- Insecure attachment. The attachment bond is the emotional connection formed between an infant and their primary caretaker. While a secure attachment bond ensures that your child will feel secure, understood and calm enough for optimal development, an insecure attachment bond can contribute to childhood problems such as separation anxiety.
Tips to reduce separation anxiety
Separation anxiety may come and go, but there’s plenty you can do to help ease your child’s symptoms. These tips can help them through this difficult period.
- Talk to your child in a calm, positive tone. Let your child know what will happen while you are gone, who they will be with and all the fun things they get to do. Even if you feel your child is too young to understand, your positive tone and attitude will send a reassuring message. It may even be helpful to find and read picture books that talk about separation and that goodbyes aren’t forever.
- Practice separating. Practice leaving your child at home with a caregiver for a short period of time. As time goes on, you can extend the time you are away before returning home.
- Ease the separation. Leave your child with their favorite stuffed animal or toy.
- Prepare an activity. Engage your child in a fun activity when the caregiver arrives or ask the daycare teacher to have an activity ready as soon as you drop your child off.
- Make your goodbye short. Whenever you leave your child or drop them off, keep the goodbye brief. If you act anxious or keep returning for just one more hug or kiss, you may unnecessarily worry your child
- Follow through on your promise. It’s important that you return when you promised to return as this helps your child build confidence and trust.
- Aim for consistency. Kids like consistency, so try to schedule the same caregiver whenever possible, so your child feels more comfortable when you leave. Develop a brief, consistent routine for when you leave to create a familiar transition from being with you to being without you.
- Attention: When separating, give your child full attention, be loving, and provide affection. Then say good-bye quickly despite their antics or cries for you to stay.
Additional tips for older children
Although separation anxiety tends to lower during adolescence, teens can experience it too. it is necessary to make sure an older child still feels safe and emotionally well to start being independent or it can resurface in untimely situations. . Here are some additional tips to help your adolescent child:
- Acknowledge their fears. Let them know you’re there for them and that uneasy feelings are natural parts of adolescence.
- Praise them for doing something they are anxious about.
- Gently encourage, don’t force, them to do things that make them anxious.
- Wait until your child is anxious before stepping in to help.
- Remind your child of times when they were initially afraid but still managed to do something.








:max_bytes(150000):strip_icc():format(webp)/avoidant-personality-disorder-4172959-5c1a913a46e0fb0001bc2c8e.png)



:max_bytes(150000):strip_icc():format(webp)/GettyImages-487729433-56f72dfc3df78c78418e35d8.jpg)
/schizotypal-personality-disorder-4689994-b8156a1551654864ab21568b0cadf60d.gif)


:max_bytes(150000):strip_icc():format(webp)/early-signs-schizophrenia-5101519_final-6861147c5e4e4a09956011952057ba72.jpg)




:max_bytes(150000):strip_icc():format(webp)/dsm-5-criteria-for-substance-use-disorders-21926_V2-c979cb0780134583bc6fa3a6f2315d63.png)








You must be logged in to post a comment.