Introduction
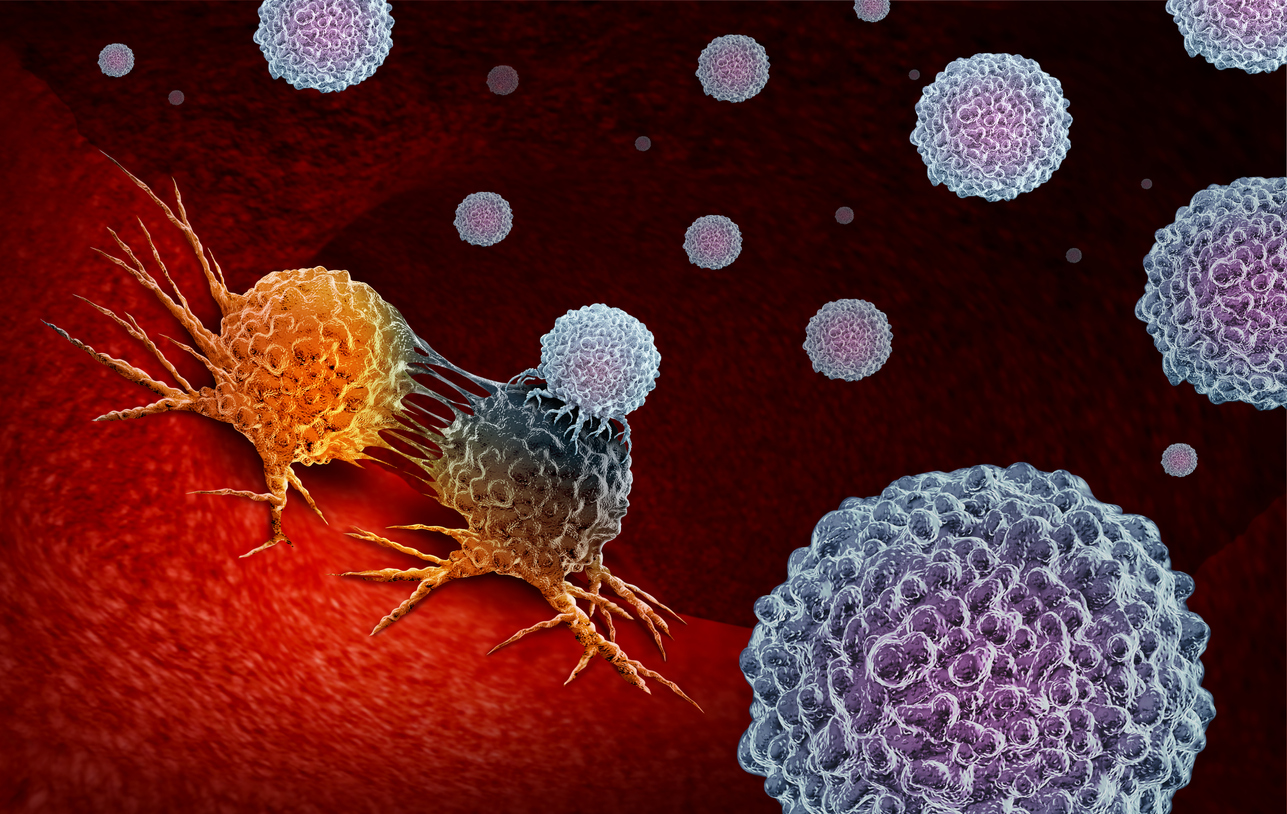
The avoidance of apoptosis by cancer cells is a prominent characteristic of cancer. Since apoptosis inhibition is at the heart of tumour growth, the clearing of malignant cells and retaining a definite number of healthy cells involves tumour-cell death. Cellular death pathway targeting provides some possible therapeutic targets for all cancers. The most obvious strategy for cancer treatment is to concentrate on lesions, particularly apoptosis in tumour cells, which eliminate cell death.
Apoptosis is an essential component of normal development. For keeping normal physiological processes between cell proliferation and cell deaths, homeostatic balance is essential. Aberrant control of apoptotic mechanisms is one of the main characteristics of cancer growth and development. Apoptosis can be activated by triggering two different molecular pathways, a pathway of the extrinsic, a death receptor or a mitochondrial pathway, intrinsic pathway also called apoptotic cascade. Extrinsic pathways from outside the cells are activated by pro-apoptotic receptors, such as CD95 and TNF-related ligands inducing apoptosis (TRAIL) interacting with specialised cell surface death receptors. Mitochondrial (intrinsic) pathways induce the transcription of or the post-translational activation of BH3 proapoptotic B-cell leukaemia / lymphoma 2 (Bcl-2) family proteins from the inside of the cell, as a result of extreme cell pressure such as DNA or cytoskeleton damaging apoptotic protease-activating factor-1 (Apaf-1) and assemblies of Cytochrome c activate caspase 9. This caspase activates the effector 3, 6 and 7 caspases, which perform apoptosis. Latest development of different therapeutic methods that interfere with apoptosis and are commonly used or studied for cancer treatment are becoming popular. It induces cancer cell death or enhances the response to certain cytotoxic medicines of cancer cells and CCs. Some of them are still in preclinical and clinical trials such as caspase activators, apoptosis modulators or agents targeting apoptosis-related proteins. Future methods for targeting apoptotic pathways in cancer patients with promising application are also seen.
Therapeutically inducing apoptosis strategies
The progressive pre-clinical or early clinical development of many therapeutic approaches inducing apoptosis are seen. The research processes two styles from a mechanical perspective of separate approach: (a) specifically separating tactics induce apoptosis, which is here called pro-apoptotic; and (b) survival-signalling techniques that modulate this to promote apoptosis, which is called permissive approach.
Proapoptotic approach:
Apoptin. A promising tumour killing technique
Apoptin (VP3) is a cell used when sparing normal cells and killing only tumour cells. The chicken anaemia virus is a source of 14,000 proteins. Latest evidence shows that this molecule induces apoptosis in which Caspases are included. Apoptin is very much shown, in vitro findings, that it is active against cancer cells without induction of natural toxicity Cells. The basic effect of it being this tumour killing only could be clarified by nuclear tumour cell location of the protein, activity requirement, whereas the protein in normal cells are Cytoplasm localised. In addition, apoptin is also active and potentially chemo resistant in genetically disrupted cells such as p53, Bcl-2 or tumour cells that express BCR-ABL. Apoptin is under progress in tumour cells in vivo in gene therapy strategies. Multiple injections of adenovirus into healthy rats or nude mouse have not been found toxic in preclinical studies. Furthermore, antitumor effects in the nude s.c. mouse were observed, hepatoma in human beings. These findings, however, remain preliminary and more preclinical work is needed with human cells to ensure safety and evaluate apoptin ‘s potential as an anti-cancer compound better.
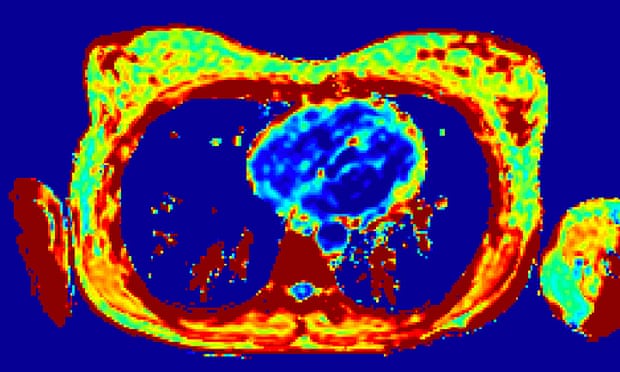
Apoptosis was examined for the development and treatment of cancer by attempting to determine its function in chemotherapy cytotoxicity caused by agents. Cytotoxic agents frequently lead to apoptotic by only a fraction of the cells. A significant portion of cells must be recruited into apoptosis to allow maximum use of apoptosis as a mechanism for anti-neoplastic agent response. The only regularly used cytotoxic agents that have been shown to induce apoptosis in breast cancer cells are paclitaxel (Taxol ®). Another of such cytotoxic agents is cyclophosphamide, and furthermore cytosine arabinoside is also used. Quantitative measurements of apoptotic cells were performed by controlling the binding of the phosphatidylserine-binding protein (FITC)-labelled annexin V into cellular cells.
Inhibitor of apoptosis protein (IAP)
The genome of baculoviruses was the original founder of IAPs because of their capacity in infected host cells to inhibit apoptosis. Re-based on the survival and XIAP of recent attempts to use IAPs to obtain anti-cancer treatment. In vitro experiments showed that the anti-apoptotic function of the proteins was inhibited by caspases-3, -7, and -9. As these cases have shown to be important in vitro for chemical apoptosis aimed at its natural inhibitors, the IAPs have been identified as a possible means of increasing chemosensitivity. In fact, NSCLC cells inhibited up to 70 per cent of surviving mRNA expression with the use of the oligonucleotide 4003, resulting in etoposide sensitization of cancer cells. Additionally, the downregulation of XIAP in ovarian cancer cells with wild type p53 by adenoviral antisense expression has caused apoptosis. These promising findings have led to clinical trials using anti-sense IAPs being mapped. The IAPs’ function may be more complex than the in vitro data initially suggested. Indeed, in NSCLC patients c-IAP1, c-IAP2, and XIAP had no precedented response to chemotherapy responses, unlike most of the expected multiple in vitro trials. Moreover, in patients with non-Hodgkin’s lymphoma and AML, there were no variations in reaction to chemical therapy between survivin-positive and negative instances. Furthermore, XIAP expression was not associated and did not have any relation with the apoptotic index of NSCLC patients but was inversely related to tumour growth. In this group of patients, higher XIAP expression has been predictively converted into a considerably longer overall survival. In addition, the nuclear localisation of survivor has shown positive effects on prognosis in a recent study of gastric cancer patients. These findings verified that it may mean that limitless ODN survival inhibition may not be desirable both within the cytoplasm and the nucleus. It is possible that the IAPs are engaged in apoptosis inhibition by the blocking of caspase but also other essential functions including proliferating. These conflicting results can be clarified. In addition, the net effect of IAPs can depend on their interaction with the control molecules Smac / DIABLO, HtrA2 and Factor1 associated with XIAP, an antagonist of the XIAP apoptotic operation. Therefore, while it is potentially promising, additional functional research and IAP interactions are required to better utilise them as goals for anti-cancer therapy.
BH3 Mimetics
There is a common consensus that BH3-only proteins are essential for apoptosis, promulgating inherent and extrinsic pathways of cell death. Based on the blocks of the sequence homology called BH domains, proapoptotic members from the BCL-2 family may be further identified. Only one domain, in general called the α-helical BH3 region is available for all BH3 protein. This preserved BH3 domain played a key role in the treatment of cancer. Three BCL-2 protein subgroups: BH3 (BCL-2 homology 3), BCL-2, BCL-2-associated X-protein (BAX), and the BCL-2 antagonist-killer (BAK), interacting on one another on the mitochondrial membrane, activate the pathway. This is the basis of three distinct groups. BH3-only proteins have been shown to achieve two mechanisms by transmitting signals to induce apoptosis, and only BH3-proteins inducted by transcriptional or post-translational cytotoxic stress. The neutralisation of antiapoptotic BCL-2 proteins or direct activation of BAK and BAX 47 is a clear way to understand the previous mode of action, both structurally and functionally, and hence the goal for production of pharmaceuticals. By attaching its hydrophobic groove by adding four hydrophobe residues it antagonises the BCL-2 antiapoptotic protein family members. Members such as cell-death antagonist BCL-2 and NOxa bind to their anti-apoptotic brothers, while other proteins such as BIM, tBID and PUMA only neutralise other anti-apoptotic agents.
miRNA
The miRNAs (MiRNAs) is a small endogenous class of 18 to 25 nucleotide length non-encoding RNAs which modify gene expression by mRNA degradation or mRNA deletion. The mature-miRNA products are produced by sequential processing by the ribonucleases Drosha and Dicer1 from a longer primary miRNA (pri-miRNA) transcript. miRNAs are known to inhibit thousands of target genes, since the objective mRNA needs only partial complementarity. Thus, one miRNA can target at the same time to a complexity of mRNAs, and several miRNAs can control the expression of one particular mRNA. The alteration of miRNAs includes a varying variety of human diseases, including cancer, by natural mechanisms miRNA are involved in number of process, including cell growth, differentiating, proliferating, apoptosis, and stem cells self-renovation. The de-regulation of miRNA also induces apoptosis avoidance, involving tumorigenesis and pharmaceutical resistance. The functioning of aberrated miRNAs, which are closely linked to the apoptosis mechanism, will act as oncogenes (OncomiRs) or tumour suppressors (TSmiRs) during tumour induction and progression. Manipulation of the levels of miRNA expression affecting apoptosis genes and pathways may also be a clinical approach to develop successful cancer treatment. Furthermore, because cancer cells frequently display a distinct trend for miRNA expression, novel profiles of altered miRNA expression may be useful for tumour-diagnosed molecular biomarkers, disease-specific outcome predictions and tumour-aggression evaluations. Therefore, numerous anti-cancer therapies are being designed to recover miRNA behaviours and rebuild gene regulation networks or drug sensitivity. A number of miRNAs were associated with drug resistance, some of them linked to apoptosis. Deregulation of miR-214 is a frequent phenomenon in ovarian cancer in human beings and it has been shown that miR-214 mainly targets PTEN / Akt pathways and promotes cell survival and cisplatin tolerance. It’s also recognised that the let-7 miR family plays an essential part in a number of cellular functions including opioid sensitivity modulation. The miRNA let-7a, aimed at caspase-3 in human cancers, was over-expressed and demonstrated resistance to a range of drugs, including doxorubicin, paclitaxel and interferon-gamma, which are caspase-3-dependent. Let-7e was up-regulated with improved tolerance to doxorubicin in some ovary cancer cell lines. Conversely, let-7i has been documented as uncontrolled in ovarian cancer resistant to chemotherapy, and the reintroduction of let-7i could sensitise ovarian resistant cell line to platinum-based chemotherapy. The cause of apoptosis induced by the chemo preventive agent curcumin has been shown to be the downregulation of miR-185 in a non-small cell-lung cancer cell line which increased its direct target expression, Caspase-10. The effect on miRNA expression profiles was thus studied by anti-cancer drugs that modulate apoptosis cell proliferation and could help predict the resistance to apoptosis. This will help prevent needless morbidity and represent a new class of biomarks to allow customised care through the awareness of possible miRNAs involved in apoptosis resistance.
Blebbishield Formation
The development of blebbishields is one method used by cancer stem cells to resist apoptosis. The emergency system is enabled to rescue the stem cells in apoptotic cancer. The apoptotic blebs merge together into a formed sphere called blebbishields. Cells undergoing blebbishield development display visual symptoms of apoptosis, but the reaction is prevented and ends in cells living. Serpentine filopodia formation due to endocytosis are involved in blebbishield formation to avoid complete apoptotic reaction. Apoptosis normally results in secondary necrosis from a lack of ATP, blebbishields by activating glycolysis are able to prevent secondary necrosis. In order to ensure clinical effectiveness, cancer stem cells must be blocked to survive in parallel to treatments by apoptosis. A variety of possible candidates were identified including inhibitors of caspase, Smac mimetics and inhibitors of the translation at an internal ribosome entrance site (IRES). IRES translation is regulated by antiapoptotic proteins, such as cIAP-2, and XIAP. IRES translation facilitates survival by converting the cIAP-2, which enflames the mechanism and moves the antiapoptotic to the proapoptotic equilibrium towards antiapoptotic survival. Hemming IRES translation will prevent blebbishield formation from being started. N-Myc is an IRES translation goal intended to avoid the development of blebbishield.
Conclusion
Apoptotic approach to seeking alternative anti-cancer drugs is intriguing, since it is not unique to the form of cancer. In both the extrinsic and intrinsic pathways of cancer there are various mutations that cause cells to evade apoptosis, which is a distinctive characteristic of cancer. A more general cancer cure will also include the opportunity to target and activate apoptotic tract. Many compounds extracted from plants that are not toxic to healthy cells are particularly promising compounds to cause apoptosis.












You must be logged in to post a comment.